Barrett’s Esophagus

Barrett’s esophagus is a disease affecting the lining of the esophagus, the swallowing tube that carries foods and liquids from the mouth to the stomach. It is caused by injury to the esophagus from the chronic backwash of stomach contents, like acid and enzymes, that occurs with abnormal reflux.
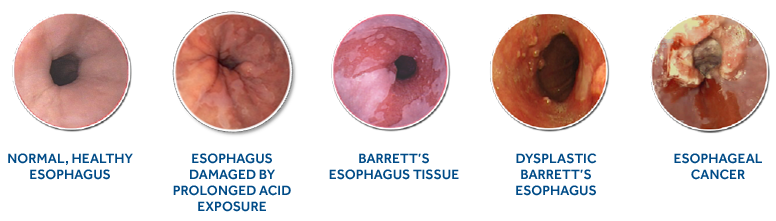
Once a person has Barrett’s esophagus, it may continually progress to more serious stages, potentially resulting in esophageal adenocarcinoma, a type of esophageal cancer. There are three stages of Barrett’s esophagus and range from the least serious (intestinal metaplasia without dysplasia) to the most serious (high-grade dysplasia). Dysplasia refers to the abnormalities of tissue or a cell that make it more cancer-like and disorganized. The presence of dysplasia is not considered cancer, but may increase the risk of developing cancer.
Cancer occurs when the abnormal cells involved in Barrett’s esophagus have rapid and uncontrolled growth and invade the deeper layers of your esophagus. This is called cancer of the esophagus, or esophageal adenocarcinoma (EAC). The cancer can also spread beyond the esophagus.
What are the symptoms?
There are no symptoms specific to Barrett’s esophagus, other than the typical symptoms of gastroesophageal reflux disease or GERD. These include heartburn, chest pain, and regurgitation.
Who is at risk?
Patients with GERD are at an increased risk for developing Barrett’s esophagus. Caucasian males over the age of 50 with chronic reflux symptoms or heartburn are also at risk for the disease.1
Being overweight (body mass index 25-30) increases a person’s risk of developing cancer of the esophagus by almost two times.2
How many people have Barrett’s esophagus?
Barrett’s esophagus is estimated to affect approximately 12.5 million adults in the United States.3
How is Barrett’s esophagus diagnosed?
For diagnosis, a physician performs an endoscopy — a procedure that allows for inspection and tissue sampling of the esophagus.
Are treatment options available?
Yes, Radiofrequency Ablation (RFA) therapy has been shown to reduce disease progression. It does this by removing precancerous tissue (called dysplastic Barrett’s esophagus) from the esophagus with precise depth control.
What happens if Barrett’s esophagus goes untreated?
In one study, 8.8% of the patients with Barrett’s esophagus and confirmed low-grade dysplasia developed esophageal cancer, which may result in removal of all or part of the esophagus.4
Esophageal cancer has a five-year death rate of 82% after diagnosis.5,6
The good news is that there is treatment available and has been shown to reduce the risk of progression to high-grade dysplasia and esophageal adenocarcinoma.
For more information, visit learnaboutbarretts.com
References:
1. Spechler SJ, Souza RF. Barrett’s Esophagus. N Engl J Med. 2014;371:836-45.
2. Turati F, Tramacere I, La Vecchia C, et al. A meta-analysis of body mass index and esophageal and gastric cardia adenocarcinoma. Ann Oncol. 2013;24(3):609-17.
3. Dymedex Market Development Consulting, Strategic Market Assessment: Barrx – GI, October 30, 2014.
4. Phoa KN, van Vilsteren FG, Weusten BL, et al. Radiofrequency ablation vs. endoscopic surveillance for patients with Barrett’s esophagus and low-grade dysplasia: a randomized clinical trial. JAMA. 2014;311:1209-17.
5. SEER Cancer Statistics Factsheets:Esophageal Cancer. National Cancer Institute. Bethesda, MD, <http://seer.cancer.gov/
statfacts/html/esoph.html> Accessed December 2015.
6. Reid BJ, Weinstein WM. Barrett’sesophagus and adenocarcinoma. Gastroenterology Clinics of North America. 1987;38:477-492.
US150791d
© 2016 Medtronic. All rights reserved. Medtronic, Medtronic logo and Further, Together are trademarks of Medtronic. All other brands are trademarks of a Medtronic company.
*Important Reminder: This information is intended to provide general information and is not a definitive basis for diagnosis or treatment. It is very important that you consult your doctor.


